During this time of economic uncertainty, the recent loss of creative, innovative leaders like Steve Jobs and Dr. Lee Lipsenthal adds to a collective national and personal concern over what seems like a serious lack of truly inventive and ethical leadership. Who will represent the next wave of 50-something leaders, and how will their personal characters influence upcoming generations?
One hope that I have for the future is Dr. Dean Ornish, a man who has been a personal friend, mentor and physician to both Mr. Jobs and Dr. Lipsenthal. To describe Dr. Ornish as a man of character, knowledge and creative medical vision would be akin to calling Winston Churchill a “good dinner speaker.”
Dr. Ornish and I have a long history of friendship, respect and support for each other’s work. Years ago, wanting to avoid being a heart surgery patient, I began to explore alternatives to legacy procedures and regimens. And, not unlike Steve Jobs, whose initial interest was also to avoid having his body violated by surgery, my research led me to the work of a young Dr. Dean Ornish. As soon as I learned more about his extraordinary program for coronary artery disease reversal, it was a simple decision to invest my own personal funds in one of his intensive workshops, held near his home in California.
As providence would have it, my own work resulted in what became a steady stream of research grants, and my subsequent personal decision to include Dr. Ornish in our appropriations for the next half-dozen years at the hospital and research institute where I previously served as President and CEO. Each year, I fought to have at least one million dollars invested in the Preventative Medicine Research Institute in California so that Drs. Ornish and Lipsenthal could continue to move forward in their research, as well.
Once, Dr. Ornish asked me, “Nick, what do you really want from our work together?” Without a moment’s hesitation, I replied, “Dean, I want to lose the question mark after the name of the town, ‘Windber.’ Whenever I tell people where we’re based, they usually respond, ‘Windber?’…’You mean Windber, PA… the old coal mining town?'” Some history here: I had been hired by the board of rural 102-bed, acute care hospital in that historic, rural community to either radically turn it around, or shut it down. For me, the latter option was never a consideration.
Among the many transformational changes we made as part of the turnaround was to be among the first hospitals — and most probably the first rural hospital — in America to implement Dr. Ornish’s evidence-based program that arrests (and can even reverse) the effects of coronary artery disease. The results — with patients of broadly diverse ethnic backgrounds — were so successful, that we were asked to present to the World Congress on Cardiology in Belgrade, Serbia in 2007 on our outcomes and research discoveries, garnered from our experience implementing the Ornish program.
We were also instrumental in introducing the program at other sites for Highmark Blue Cross, as well as a host of other innovations and reforms at our own hospital; from live music playing, to fountains, delicious, nutritious food, cooked by classically-trained chefs, 24-hour family visitation and… wait for it… pajama bottoms for the comfort, dignity and modesty of our patients.
The goal: an environment entirely dedicated to the healing of body, mind and spirit.
The result: among other verified successes, one of the lowest hospital acquired (i.e., nosocomial) infection rates – less than 1%) in the U.S., where the national average is around 9%.
And, yes, we were profitable. Consistently profitable, quarter over quarter.
On one flight in a private plane with my board chairman and me from Cincinnati, Dr. Ornish and I had mutually planned to spend some “quality time” together – collaborating, planning and just trading stories about our experiences. Instead, he wound up honoring an emergent commitment as a personal health advisor and consultant to the leader of an Asian nation, and spent the majority of our flight in direct, one-on-one communication with this person. Awesome? That’s just the kind of guy he is.
My personal hope is that Dean Ornish will take up the mantle for both Jobs and Lipsenthal, as he takes his wellness programs to new levels through mobile apps and enterprise solutions using iPhones and other mobile devices, and iPads and other tablets, making innovative use of social media technology. (Talk to my friend Mike Russell about that.) My further hope is that Dr. Ornish’s success as an agent of influence and change will continue to be used in a powerful way, to not only help improve the health of the world, but to continue to positively influence public policy in the United States, as well.
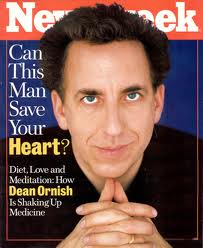 Dean Ornish has long been recognized as a leader, a man of character and a visionary, but with the loss of two of his closest friends, the pressure to perform grows exponentially greater. So, my best to you Dr. Ornish. Thanks for your confidence in my work. Keep the faith, and keep up the good fight to make a phenomenal difference in this world, thinking in insightful new ways and never resting on your laurels. As your friend Steve Jobs famously said at his Stanford commencement address, “Stay hungry. Stay foolish”…but especially the phrase he immortalized early in his career: be “insanely great.”
Dean Ornish has long been recognized as a leader, a man of character and a visionary, but with the loss of two of his closest friends, the pressure to perform grows exponentially greater. So, my best to you Dr. Ornish. Thanks for your confidence in my work. Keep the faith, and keep up the good fight to make a phenomenal difference in this world, thinking in insightful new ways and never resting on your laurels. As your friend Steve Jobs famously said at his Stanford commencement address, “Stay hungry. Stay foolish”…but especially the phrase he immortalized early in his career: be “insanely great.”














 He then challenged the other Boston hospitals to do the same. He was accused of self-aggrandizement, egomania, and numerous other witchcraft-like things, but the bottom line was that the number of infections went down, and they went down because the staff and employees wanted to do better and wanted them to go down.
He then challenged the other Boston hospitals to do the same. He was accused of self-aggrandizement, egomania, and numerous other witchcraft-like things, but the bottom line was that the number of infections went down, and they went down because the staff and employees wanted to do better and wanted them to go down.