Nick Jacobs, among his other affiliations, is an officer of the Integrative Health Policy Consortium, which represents more than 600,000 IHM practitioners; president of the Clinical and Translational Genome Research Institute, which he founded; and a consultant to the Department of Defense in breast cancer research.
•
Pennsylvanians received good news recently when the Pennsylvania Health Care Cost Containment Council reported that hospital readmissions and mortality rates continue falling locally and statewide.
The report shows these rates declining for a number of common types of treatments. It gives much of the credit to a “commitment of PA hospitals to provide quality care” and to the Affordable Care Act, which ties reimbursements to that quality care. This, in turn, encourages health care facilities to strive for improved mortality rates because doing so helps keep government funds flowing through their doors.
Regardless of the motivation, this is good news. But it’s not good enough.The mortality rate could be improved even more dramatically if more healthcare administrators and physicians would introduce integrative health and medicine practices into their services.
Integrative health and medicine (IHM), as defined by the American Board of Integrative Medicine and the Academic Consortium for Integrative Medicine & Health, recognizes the importance of the relationship between practitioner and patient. IHM focuses on the whole person, is evidenced-based and employs a wide range of appropriate therapies, healthcare professionals and disciplines to achieve optimal health and healing.
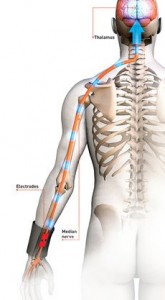
Integrative health practice includes treatments and therapies such as acupuncture; natural products; deep breathing; Tai chi and Qi Gong; meditation; massage; special anti-inflammatory diets; progressive relaxation; journaling; biofeedback; pet, music and dance therapies; hypnosis and guided imagery. When provided by a licensed or certified health care professional, IHM provides numerous benefits. It can decrease chronic pain, post-operative pain and the need for medications. It can improve patient satisfaction and shorten hospital stays. It can lower mortality rates. IHM methods also are relatively inexpensive.
Many places, including the Cleveland Clinic, have reported cost savings per patient, while also seeing reductions in patient anxiety, pain, and medications. During my tenure as CEO at Windber (Pa.) Medical Center, I worked with physicians, staff, and volunteers to create a healing environment by embracing all methods and therapies used in integrative medicine and combining them with the ambiance of a fine hotel and the amenities of a health spa. We carefully scrutinized and credentialed practitioners specializing in services such as aroma and massage therapy, integrative nutritional counseling, acupuncture, chiropractic manipulation, pet and music therapy, reiki and spirituality, to name a few.
In short, a healing environment permeated our facility.
Yes, we had our share of naysayers and opposition among physicians, allied health care professionals and others, but over time our infection rate dropped below 1 percent and stayed there for a decade. (The national average is 9 percent.) Of our peer hospitals, we had the lowest readmission rates, restraint rates and lengths of stay. Even with a palliative care unit to care for dying patients and their families, we had the lowest death rate among our peer hospitals.
For those who would say it was all coincidence because Windber is a small hospital, I would direct them to the 19,000 papers written supporting the efficacy of acupuncture alone, and then to the thousands of papers written about the healing power of music, massage and so many other treatments dismissed all too readily by traditional practitioners.
IHM practices are not at odds with traditional medical practices; rather, they enhance them. Yet in many hospitals and physicians’ offices, they are ignored, discouraged, even ridiculed. Such negative reactions result from ignorance, misinformation, prejudice and even greed — pharmaceutical companies, for instance, see no profit in promoting most IHM treatments, and some medical practices might earn less if, instead of scheduling patients for costly treatments or surgeries, they instead treated patients with acupuncture, spinal manipulation, massage therapy or even mindfulness.
Resistance to IHM is breaking down, but this shift in attitude needs to be accelerated. If you travel to Europe or Asia, you will see integrative medicine practices thriving because their value is acknowledged and embraced. In America, IHM beachheads are being established in health care systems and universities, thanks to such groups as the Family Medicine Education Consortium, Integrative Health Policy Consortium and the Academy of Integrative Health and Medicine, of which I am a co-founder. The academy includes among its member’s hundreds of licensed physicians who have successfully merged IHM with traditional medical practices.
Much remains to be done to more broadly spread the healing benefits of IHM, which will happen only when more patients take more responsibility for their health and demand IHM treatments, more physicians research and adopt them, and more insurance companies pay for them. When that day comes, there will be a lot more good news about mortality rates and other measures of medical care for Pennsylvanians and people all over the country to celebrate.